Microbiome, Diet, Health, and Disease: Policy Needs to Move Forward
This article covers policy needs concerning the rapidly evolving field of microbiome and diets with respect to health and disease. It captures some key outcomes of a multi-stakeholder dialogue (Brussels, May 2016), spearheaded by a joint effort of the Organisation for Economic Co-operation and Development (OECD) and the Department of Economy, Science and Innovation of the Flemish Government (Belgium), to help design and/or interpret regulatory frameworks for food and drugs to support innovation to benefit society, while guaranteeing safety and efficacy of products and ensuring the science base.
Introduction
The combined genomes of the microbial ecosystems that live in symbiosis or as commensals with the human body can be defined as the human microbiome. These microbial ecosystems not only include bacteria and archaea, but also fungi, protozoa, and viruses. Different microbial ecosystems colonise the mouth, the skin, the vaginal and intestinal tract, of which the latter has the highest biodiversity, composed of more than 1000 phylospecies.An Interface Between Human Genetics and Diet: the Gut Microbiome
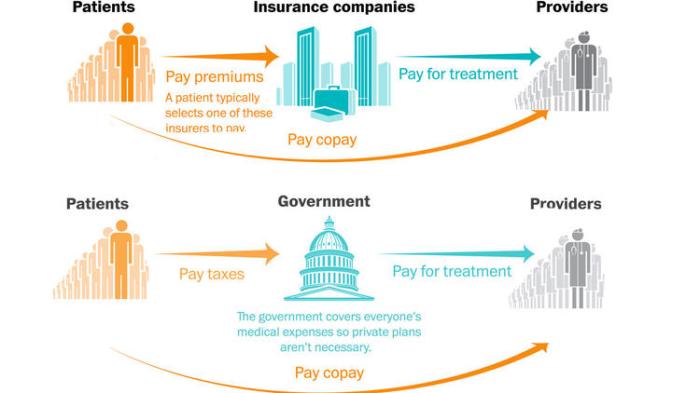
The human gut microbiota has been described as a key biological interface between human genetics and environmental conditions, such as diet, that can modify the composition and the functioning of the intestinal microbiome. In that sense, it may be considered a virtual organ which is an integral and essential part of the body.1 Through nutritional intervention, the gut microbiome may be altered to generate better wellbeing and protection against many diseases or even to cure certain conditions.2-4The gut microbiome can be linked to many Non-Communicable Diseases (NCDs), such as cardiovascular diseases, cancer, diabetes, and metabolic syndrome related to increasing incidence of obesity. More recently, also neurological diseases have been related to gut microbiota and diet and are considered as NCDs.5, 6 The burden of ageing related dementia and other NCDs is exponentially increasing in relation to changing life styles and ageing of the population, conditions that are associated with gut microbiome alterations. Changing demographics worldwide, combined with the broader adoption of the western diet and lifestyle increases the burden of NCDs, creating serious challenges for the public healthcare systems. Prevention and more efficient treatment of NCDs not only offer important economic advantages for healthcare systems, it also contributes to the reduction of poverty as only healthy people can actively participate to society and economies.7-9 Recent scientific studies are linking dietary habits to an array of health conditions in new ways and indicate that nutrition has a determining influence that start even before birth and can influence the development of complex pathologies.10, 11
Opportunities and Hype
New insights about the importance of the intestinal microbiome and the modulating effect of diet are opening new possible ways of treatment and prevention that may contribute to the sustainability of healthcare systems by keeping the increasing healthcare costs under control. Innovations based on better understanding of how the intestinal microbiome functions and regulates our health and how it is impacted by what we eat are expected also to lead to preventative medicine and contributions to longer wellbeing in general.However, the field is subject to some hype. Although insights are growing fast, at this moment it is still unclear how health or disease is determined by the human microbiomes. In most cases, a certain microbiome composition can at best be associated with certain condition. The causal relation of nutrition, gut microbiome composition and health is not clearly understood yet, such as whether a healthy microbiome can be defined at population level, what determines its resilience when disturbed, or how its composition can be beneficially manipulated. Such primary knowledge is required before therapies targeting the microbiome can be developed.
Nevertheless, there is a clear interest of food and pharmaceutical developers and industries to develop new products that target the gut microbiome, for better well-being or to manage chronic disease conditions. Moreover, microbiomes are also a source of novel bioactive compounds that may be used for innovative applications.
Identifying Policy Needs
To follow the pace of new scientific insights and translate these to innovative applications, there is a need to accelerate policy actions at the national and international level, to address scientific and regulatory challenges as well as to ensure safety and efficacy and efficient take up by consumers and healthcare professionals.12-14To stimulate innovation based on the new insights of how the human microbiome and the gut microbiome in particular is functioning, in May 2016, the department of Economy, Science and Innovation of the Flemish Government in Belgium organized a workshop on ‘The Microbiome, Diet and Health: Assessing Gaps in Science and Innovation’ in Brussels in collaboration with OECD and the Business and Industry Advisory Committee (BIAC), the industry association linked to OECD.15
This workshop brought together scientists from academia and industry, experts in regulatory issues and policy makers to identify and discuss on policy needs for this field to progress and deliver upon the promises. The regulatory frameworks in place need to follow fast the new developments and combine a right balance between measures to ensure safety and consumer/patient protection and flexibility to adapt to these new developments.16-18
This article summarizes some of the policy needs that were identified as well as messages from workshop participants, how to address these and help move from hype to solid intervention or prevention. A complete workshop report is published by OECD.
continue
Labels: Become Compliance Expert, Drugs and Biologics Courses, FDA Regulation Training, Food Compliance Courses, Healthcare Compliance Professional Courses, Medical Device Courses, Online Professional Courses